You may be invited to engage in contact tracing if you test positive for the COVID-19 virus — or if your doctor believes you have the virus but has not received test results yet. Contact tracking is critical for minimizing infectious illness transmission. Contact tracing is more efficient in limiting viral transmission the sooner it begins.
To begin, you supply a list of individuals with whom you had close contact during the period you were possibly infectious. Public health officials then contact those close contacts to inform them of the exposure and their risk of infection. Your identity is safeguarded during this information exchange.
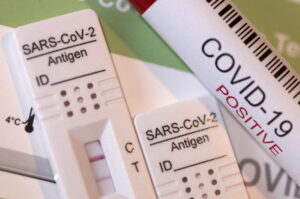
The contact tracing team gives guidance on how close connections may help reduce the risk of viral transmission. Following an exposure, steps may include having a COVID-19 rapid antigen test, keeping at home and away from people — a process called quarantine — learning about signs and symptoms, and taking further measures.
Suggestions for quarantine
Whether you have had intimate contact with someone who has COVID-19 and is not completely vaccinated, isolates yourself for five days after the exposure to see if you acquire COVID-19 symptoms. Then, for a further five days, wear a mask. If quarantine is not possible, use a mask for ten days. Keep a safe distance from members of your home. Self-isolate if you are experiencing symptoms. learn more about COVID-19 symptoms at https://www.cdc.gov/coronavirus/2019-ncov/symptoms-testing/symptoms.html
If you have had COVID-19 in the previous three months or have had all recommended vaccination doses, including boosters and extra main injections, you are normally not required to quarantine. However, for ten days, wear a mask.
If you have gotten the required vaccination doses but not a booster, you should remain at home for five days. After at least five days, get your blood checked. And continue to wear a mask for another five days. If you are unable to remain at home for ten days, use a mask.
Coronavirus Rapid antigen tests Made Simple (PCR Rapid antigen tests)
To confirm the presence of the SARS-CoV2 coronavirus in the upper respiratory tract in people suspected of having COVID-19, a potentially painful nasopharyngeal swab collection (PCR analysis for genetic viral material) is frequently performed. With careful preparation and pre-medication before to the coronavirus rapid antigen tests, this sort of coronavirus test may be less uncomfortable.
How Is Coronavirus Testing Performed (PCR Swab)?
The testing technique itself involves inserting a swab coated with an absorbent substance approximately 3 inches into the nose and into the back of the throat. The swab is then swirled for about 15 seconds before being withdrawn. The New England Journal of Medicine has produced a handy video on how to do coronavirus testing using the swab approach.
Due to the fact that the nose is not used to having an instrument inserted within, the majority of individuals find this operation to be psychologically unsettling and physically quite unpleasant. Indeed, if you do not feel any pain throughout the operation, the rapid antigen tests were probably not performed properly, resulting in incorrect findings.
Is Coronavirus Rapid antigen tests (PCR) Involved in Pain?
Numerous feelings may occur during coronavirus PCR rapid antigen tests. Transient discomfort, intense burning within the nose, choking when the back of the throat is touched, sneezing, coughing, and tears have all been recorded as a result of the nasal lacrimal reflex being triggered. If you have a considerable septal deviation or clogged nasal passages as a result of allergies, cold-like symptoms, or nasal polyps, passing the nasal swab to the back of the throat may be extremely difficult.

How Can I Reduce the Pain in My Nose During the Coronavirus Rapid antigen tests (PRC)?
One strategy that may simplify the surgery is to simply administer a topical nasal decongestant (0.05 percent oxymetazoline, brand name Afrin) into the nose 30 to 60 minutes before to the treatment. One drop in each nostril administered while laying down is typically sufficient to decongest the nose enough so that the nasal airway is maximally dilated when the swab is passed. This may help prevent the swab from pressing on the nasal tube walls, causing discomfort and sometimes bleeding. By the time the swab is obtained and the coronavirus rapid antigen tests are completed, very little residual oxymetazoline is remained in the airway to impair virus viability or interfere with the assay. Additionally, taking an antihistamine 30-60 minutes before the test may help avoid or alleviate sneezing, coughing, and tears.
Facilitating the collection of nasal secretions through a nasopharyngeal swab may boost patient acceptance and result in higher-quality specimens for rapid antigen tests.
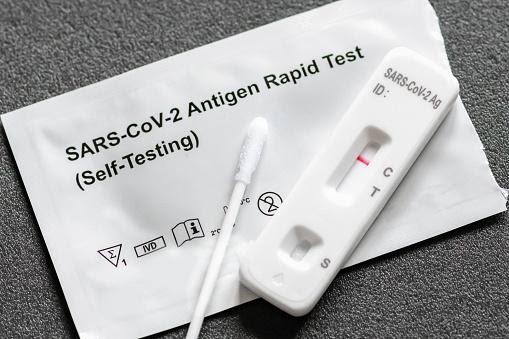
Now, more than two years into the epidemic, at-home quick tests are accessible to the general public and are a critical component of many communities’ infection-control strategies.
However, when customers do their own COVID-19 rapid antigen tests at home, the possibility of an erroneous result exists if the rapid antigen tests are not given appropriately. There are effective testing methods, which we discuss below with the assistance of infectious disease expert Dr. Douglas MacQueen.
• Step 1: Verify the product’s expiry date.
• Step 2: Conduct a search for any recalls associated with the rapid antigen tests you are administering. You may do so by visiting the website of the Federal and Drug Administration here.
• Step 3: Wash your hands and disinfect the testing area. “There is a potential that you have viral particles or another virus on your skin that cross-reacts with that antigen test,” Dr. MacQueen says. Let’s say you’re collecting it and come into contact with the swab; this could result in a false positive result on the test, meaning you don’t have COVID-19 but do have another coronavirus on your hand from wiping your nose or your child’s nose and then getting it on a swab, which the test detects.”
• Step 4: Before delivering the exam, carefully read all instructions.
• Step 5: Organize the contents of your rapid antigen tests kit.
• Step 6: Identify the kind of nasal swab and the duration of the procedure in the instructions. Dr. MacQueen states that there are often “two options: one is a swab inside your nose, which is bearable. The other is buried deep inside your nostrils. If the exam you purchased requires you to do so, I urge you go as far back as feasible. Whether it’s back in the nose or just in front of the nostril, rotating the swab three or four times or whatever many times the manufacturer recommends in your kit is typically necessary to attempt to capture any virus particles present on the swab. Some of them may advise you to blow your nose ahead of time if you have mucus discharge or a runny nose.”
• Step 7: Comply with the time constraints associated with each step of the rapid antigen tests and pay careful attention to the findings. “Interpreting the data might be challenging,” Dr. MacQueen explains. Many of them describe it like a pregnancy test when a little band begins to change color. If anybody has been through that, deciphering the pregnancy test and determining if it is positive might be a little challenging. Therefore, there are occasions when it is necessary to wait a short period of time and allow the line to completely grow on these COVID rapid antigen tests.”